I already have a diagnosis of a psychiatric disorder, how might a crisis or disaster affect me and what should I do?
If you’ve been diagnosed with a mental health condition, it’s important to know that the stress associated with a crisis might cause your symptoms to worsen. We encourage you to take the following steps to look after your emotional health.
- If you are currently receiving treatment, be sure to continue with that treatment. If you are not able to receive in-person care, develop a plan for telehealth sessions with your provider(s).
- Make sure that you’re taking your medications as prescribed and have a plan for maintaining access to those medications.
- If you are not currently receiving treatment, make sure to monitor your symptoms closely and reach out to your mental health care provider(s) if those symptoms begin to worsen or impact your daily life.
- Think back to the strategies and coping skills that were helpful to you in the past and put them back into action now.
- Find additional mental health supports.
I am worried about my mental health but have never had significant mental health problems. Am I at risk of developing a mental health disorder because of stress from a disaster?
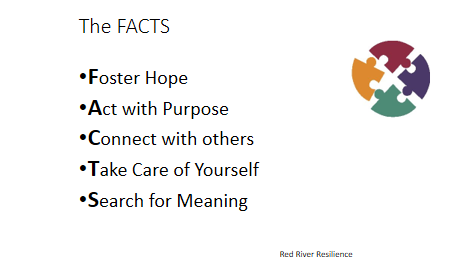
Disasters can be very stressful for individuals and communities, particularly for those who suffer significant losses, or are directly impacted by the event. Many will experience symptoms related to mental illness, such as anxiety, depression, stress, etc… but for most, they are short lived. A smaller group of individuals will meet criteria for a diagnosis of a mental illness. While not a guarantee against more serious concerns, individuals and communities can practice and build their resilience. The acronym FACTS can be a helpful reminder:
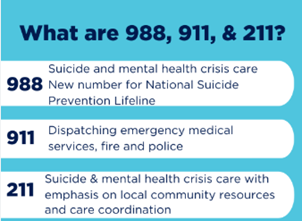
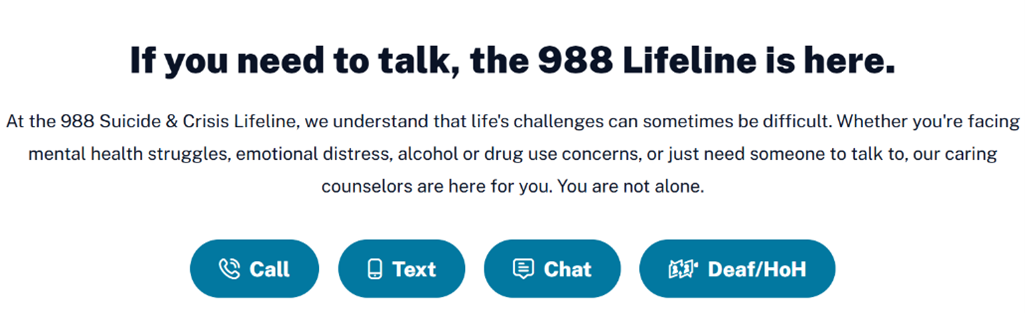
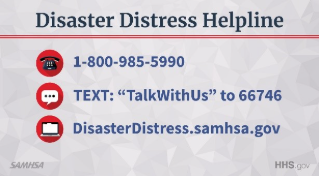
And, unfortunately, there are more frequent natural and human-caused disasters (large scale events disrupting community functioning) occurring. As such, there is year-round crisis-counseling available through the following resource:
Learn more about each of these common behavioral health concerns, and review a list of common symptoms.